Five tips for young people dealing with long COVID – from a GP
Dr Dipesh Gopal from Queen Mary's Wolfson Institute of Population Health has written for The Conversation giving advice for young people with long Covid.

General practitioner reassuring a patient. Credit: iStock.com/AJ_WATT
While we might not be hearing the daily COVID numbers anymore, the virus hasn’t gone away. In the UK alone, thousands of new cases continue to be recorded every day.
Meanwhile, there’s a very large group of people for whom the virus hasn’t gone away in a different sense – those suffering with long COVID. For these people, symptoms persist after the infection itself has passed (technically, beyond 12 weeks after infection).
The most common long COVID symptoms include fatigue, breathlessness and loss of sense of smell. But people experiencing long COVID report a whole range of symptoms.
Long COVID symptoms
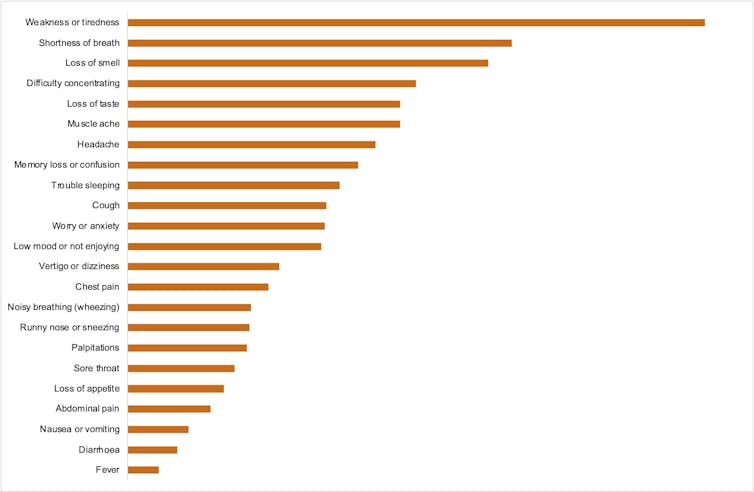
For many people with long COVID, their symptoms affect their ability to live and work normally. Symptoms can last a few weeks for some people, while for others, they can go on for much longer.
We don’t fully understand why long COVID happens, but one theory is that it’s due to an over-reaction of the immune system or the blood vessels.
Between 3% and 12% of people who get COVID go on to develop long COVID. About 2% of people in the UK are currently experiencing long COVID.
Data indicates women are more likely to develop long COVID, and people aged 35 to 49 are most likely to experience symptoms compared with other age groups. Having certain health vulnerabilities, such as a compromised immune system, also makes people more susceptible. This doesn’t mean other groups such as men, children and young adults can’t be affected.
In fact, around 250,000 people aged between 17 and 34 in the UK are estimated to have long COVID at the moment. Notably, many young people with long COVID probably haven’t experienced living with a long-term illness, and so may not be familiar with navigating the healthcare system, which can be tricky.
I’m a GP and these are my top tips for what to do if you think you might have long COVID.
1. Recognise if your symptoms need urgent attention
If your symptoms seem potentially serious, don’t delay seeking medical attention. If you have symptoms such as persistent chest pain, palpitations, breathlessness or confusion, or you’re unable to speak or move your arms or legs, you should get help via the emergency department or 999. Otherwise, proceed with the following steps.
2. Register with a GP
If you’re not registered with a GP practice, do this as soon as possible. Access to primary care in the UK is free regardless of immigration status. But not all hospital treatment is free for everyone.
3. If you have symptoms, contact your GP
I know this can be frustrating – I find it hard to get an appointment with my own GP. If you have the energy, call the practice early in the morning. If you’re offered a telephone appointment, take it, and you may be offered an in-person appointment later.
If you can’t get through on the phone, fill in the online form with your concerns if your GP practice offers this on their website. If you still can’t contact your GP practice after trying at different times of day in the same week, you might consider moving to another practice.
4. Have an idea of what you want from the appointment and be prepared
What are you worried about? Would you like to be examined? Do you need your doctor to sign you off from work? Be clear with what you’re expecting and hoping to get from the appointment – this will help the appointment run as smoothly as possible. It can be a good idea to write a list and talk through this with your GP at the beginning of the appointment.
At the appointment, a few things might happen. You might be asked questions about your symptoms or asked to fill in a questionnaire. If you can wear easily removable clothing, do so, especially if you’re likely to be examined. For example, if you’ve been feeling breathless, wear a loose-fitting shirt as the doctor will probably want to listen to your chest.
You may be offered blood tests, an ECG (which checks the heart rhythm), or even a chest x-ray to investigate what may be causing your symptoms. After this your case details might be sent to the local long COVID clinic or for review by a team of experts (called a multi-disciplinary team) where you might undergo tests and treatment not available at your GP practice.
5. Seek out other resources
You might find it helpful to visit the NHS COVID Recovery website or access long COVID support resources online. These provide links to patient forums, support services and symptom-specific advice.
There may be a role for non-medical therapies such as yoga and drama too, although there is limited evidence to show these can support people with long COVID. Interestingly, a recent study found that a six-week breathing programme run by opera singers improved mental health, though not physical health, for people with long COVID.
A final word
In our clinic, we’ve observed that people who didn’t rest while they were acutely unwell with COVID and immediately afterwards have been more likely to develop a more severe version of long COVID. This observation has been backed up by recent survey data.
So rest while you are unwell with COVID and even once you recover, especially if you can afford to do so.
This article first appeared in The Conversation on 20 May.
Related items

11 December 2024

5 December 2024

2 December 2024