Hard graft: How Queen Mary research created a landmark range of synthetic bone-graft materials
In collaboration with
Hailed as one of the most important feats of British engineering in the last 50 years, Queen Mary researchers developed a range of cost-effective synthetic bone graft materials. These innovative products are more effective than the current standard treatment – and patients don’t have to undergo risky additional surgery to harvest donor tissue.
This research brought together a wide range of scientists and academics across the University and other institutions. They are listed in full below.
When bones fracture, they can often remodel and heal themselves. But sometimes the fracture is too big or complex for the bone to repair without help, so surgical bone grafts are needed. The graft acts as a scaffold, supporting the patient's own bone cells to use the graft as a conductive surface to bridge any large gaps and heal the break.
Bone grafts can be either taken from the patient’s own body (an autograft), from a donor’s body (allograft) or are engineered (ie a synthetic material).
What risks do bone graft operations carry?
An autograft introduces the patient’s own living ‘bioactive’ bone tissue into the area. It usually involves two procedures in one operation: first to harvest the bone, then another to implant it. The need for a second operative (donor) site increases the length of the operation and the infection risk and in some cases patients suffer from long-term discomfort at the donor site. Moreover, the amount of bone that can be safely harvested is limited.
While donor site complications and supply issues are eradicated with the use of allograft, these procedures carry a risk of immune rejection. Furthermore, in allografts, the donor bone also has to be treated and sterilised before it can be used, which reduces its bioactivity or capacity to support bone regeneration and healing.
In contrast, not only are supply issues eradicated for synthetic bone grafts, but the immune rejection risk is virtually zero. Furthermore, if a synthetic graft can be engineered to have the same or better bioactivity as autografts then both safety and efficacy is improved, resulting in not only a significant reduction in patients encountering complications that delay their recovery or require further surgery, but also in reliably faster healing.
How do synthetic bone grafts work?
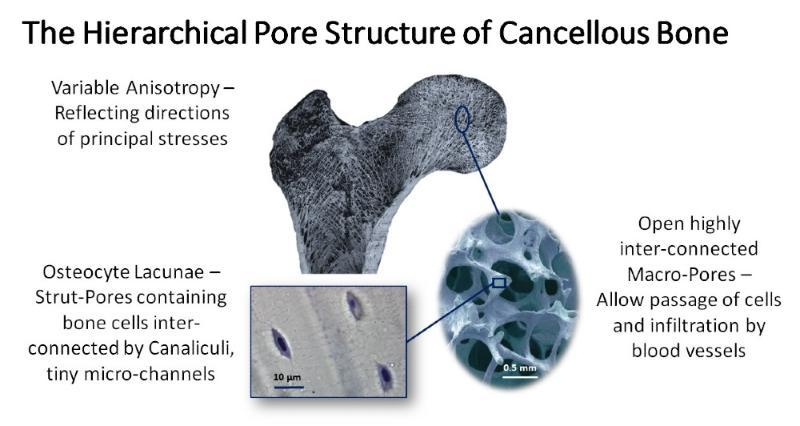
Synthetic bone grafts are made from highly porous materials (such as usually ceramics-based), and have an open, foam-like structure. This structure mimics the spongy internal tissue of our bones (which is called cancellous bone). A synthetic bone graft stimulates the patient’s bone and stem cells to form new bone tissue.
Initially, this regenerated bone tissue incorporates the synthetic bone graft, but with time both the new tissue and scaffold may be remodelled and replaced with new more mature bone as part of the bone’s constant cycle of regeneration and renewal.
Early synthetic bone grafts were often unreliable and ineffective. Less was known about the body’s biological response to these synthetic materials and the need for these materials to work synergistically with the host to support healing or to have the capacity to be remodelled in the longer term.

The ‘in theatre’ image shows Inductigraft™ packed into a vertebral spacer. The Inductigraft™ X-ray image reveals the inductigraft in between the two vertebrae.
What did the researchers do?
An earlier team of Queen Mary researchers, led by Professor William Bonfield and Professor Serena Best (in collaboration with Dr Hing and Professor Iain Gibson), studied graft chemistry and structure to develop new, improved synthetic bone grafts. This distinctive expertise led to the foundation of the QMUL spinout ApaTech in 2001, to commercialise this novel technology and launch the synthetic bone grafts ApaPore™ (2001) and Actifuse™ (2005) for clinical use. The company was acquired by Baxter International in 2010.
Since 2000, Dr Karin Hing has built on this pioneering research, studying the mechanisms behind the sensitivity of bone healing to the chemistry and structure of synthetic bone grafts. Her team found that, in addition to having the right chemistry, the ability of a synthetic bone graft to stimulate bone regeneration was particularly sensitive to the physical or structural composition of the graft. In particular, the level of porosity and the presence of tiny interconnected ‘micropores’ – half the width of a hair – within the struts surrounding the larger pores.
The material’s pores are vital: Just like natural bone tissue they have a hierarchical structure, the larger pores need to be the right size for new bone to grow into – and interlinked to allow the exchange of cells and nutrients via blood vessels to nourish and sustain healthy bone tissue. The presence of the tiny interconnected pores within the struts enhances rapid nutrient exchange, improving the graft’s bioactivity.
This research resulted in the UK launch of the synthetic bone graft material Inductigraft™ (or AltaPore™, as it’s known in the US) in 2013.
Why is Inductigraft™ so important?
Dr Hing’s results and subsequent clinical trials showed that Inductigraft™ could be just as effective as an autograft with a significant advantage – the patient wouldn’t need additional surgery to harvest the autograft. Mr Robert Lee, Consultant Orthopaedic and Spinal Surgeon at the Royal National Orthopaedic Hospital Stanmore, said this eliminates “the associated risks of infection, pain and complications” of such surgery.
Making surgery shorter and safer
As patients are less likely to need additional surgery, there’s a reduced need for anaesthesia – so fewer surgical risks for the patient. Also because there’s no need to harvest autograft bone the operation is shorter, with patients anaesthetised for less time.
Secondly, a patient treated with Inductigraft has less chance of needing revision surgery because “the excellent fusion rates significantly contribute to the improvement in patient reported outcomes,” according to Mr Lee. A result endorsed by Mr Michael Mokawem, Consultant Spinal Surgeon, Royal National Orthopaedic Hospital NHS Trust who reported an impressive 98.9 per cent fusion rate in surgery. Moreover, patients were typically released from hospital two to three days earlier, improving quality of life for the patient and reducing healthcare costs.
Helping patients heal quicker and better
In the longer term too, Inductigraft™ helped bones continue to make a full recovery after the initial fusion: Mr Mokawem noted that CT scans twelve months after surgery showed “close to 100 per cent fusion (only one out of 150 was not fused), whereas for other synthetic bone grafts it would be 80-92 per cent.” He suggested that one of the reasons for Inductigraft’s more reliable results was that the better pore structures improve blood flow through the bone tissue.
In clinical trials at 12-months post-fusion, motor, sensory functions, reflexes, straight leg raise and femoral stretches were also either maintained, or better in over half the patients. Patients also said that, following their surgery, they were in less pain and life had improved post-surgery.
Importantly, unlike traditional growth-factor based treatments, Inductigraft™ is suitable for children or adolescents, making successful outcomes more likely for them.
Together, Actifuse™ and Inductigraft™ have transformed the lives of hundreds of thousands of people globally: over 400,000 patients in 30 countries to date.
Actifuse brings the same extraordinary results to knee injuries
In 2005, Baxter launched Actifuse™. Its use has since expanded from its original application in spinal injuries to use in knee-surgery, with similarly transformative effects. Not only did Actifuse™ halve the operation time (64 minutes as opposed to the 114 minutes needed for the average autograft operation), the study also found that the Actifuse™ group were free of complications.
Stamp of approval
The landmark development of Actifuse™ and Inductigraft™ bone graft substitutes was recognised in 2019 with the issue of a Royal Mail stamp. The stamp was released as part of a series celebrating seven of the outstanding British engineering achievements of the last 50 years.
Cost-effective and reliable
Together, Actifuse™ and Inductigraft™ have transformed the lives of hundreds of thousands of people globally: over 400,000 patients in 30 countries to date, with the grafts used in around 24,000 operations a year. The materials have been a huge commercial success and currently account for around one per cent of the global bone graft substitutes market (worth an estimated $3.78 billion in 2022). A feat of engineering that improves life daily for people around the world.
Researchers
Key researchers on this project included:
Professor of Materials Science, University of Cambridge
Emeritus Professor of Medical Materials, University of Cambridge
Theme Professor (Health and Wellbeing), University of Portsmouth
Professor of Medicine, University of Central Florida
Professor of 3D X-ray Imaging, Institute of Dentistry
Personal Chair, University of Aberdeen
Professor Doctor of Science, HAZU
Professor Peter Revell
Professor Emeritus, University College, London
Professor of Inorganic Chemistry, School of Biological and Chemical Sciences
The following researchers worked on the project as part of their PhD studies:
- Dr Basil Annaz
- Dr Viviana Castagna
- Dr Navinderpal Chana
- Dr Mouna Chetehouna
- Dr Katharina Guth
- Dr Dinara Ikramova
- Dr Jasmin Köhnken-Sawall
- Dr Krystelle Mafina
- Dr Alan Parish
- Dr Sophie Parsons
- Dr Nelesh Patel
- Dr Sorousheh Samizadeh
- Dr Feng Yang

